Trying to suture or staple a scalp laceration is oftentimes a hairy proposition for emergency physicians who repair these types of wounds regularly. Although the “hair apposition technique” method is one option, if one opts for sutures or staples, the most difficult part of the procedure is trying to avoid trapping hair strands within the wound, which may cause wound dehiscense, a foreign body reaction, or a local infection.
Trying to suture or staple a scalp laceration is oftentimes a hairy proposition for emergency physicians who repair these types of wounds regularly. Although the “hair apposition technique” method is one option, if one opts for sutures or staples, the most difficult part of the procedure is trying to avoid trapping hair strands within the wound, which may cause wound dehiscense, a foreign body reaction, or a local infection.
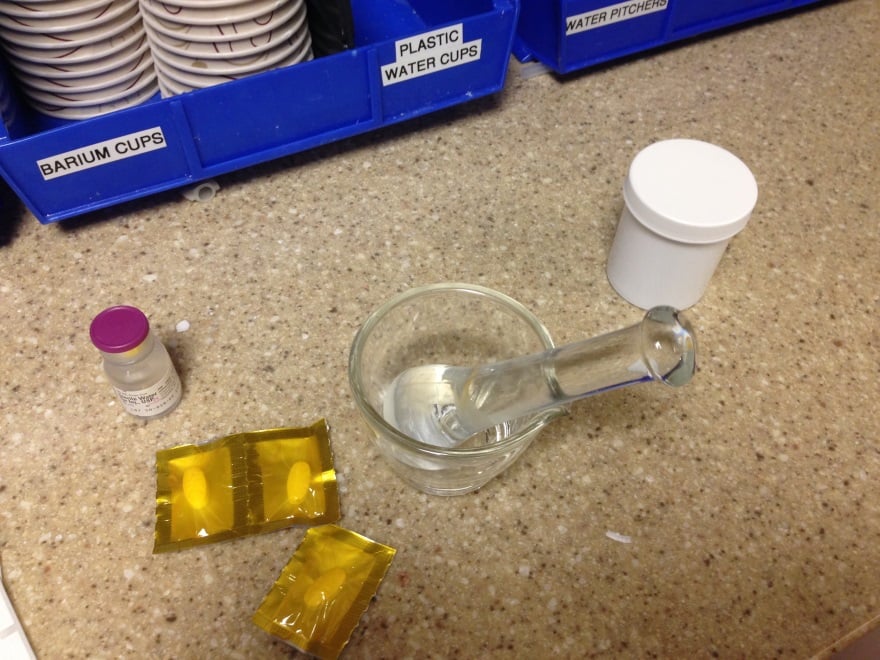
Trick of the Trade: Part the hair away from the scalp laceration with petroleum-based jelly

A useful solution to this problem is through the use of a thick petroleum-based ointment to displace the hair to each side of the wound. Bacitracin or similar topical antibiotic derivatives can be used, as can petroleum jelly.
Author information
The post Trick of the Trade: Parting the hair for scalp laceration repair appeared first on ALiEM.






























































 Jacob Avila, MD RDMS
Jacob Avila, MD RDMS

 Melissa Barton, MD
Melissa Barton, MD Ciara Barclay-Buchanan, MD
Ciara Barclay-Buchanan, MD Mark Favot, MD
Mark Favot, MD An 82-year-old female is brought into the Emergency Department by family for a several day history of progressive altered mental status. You initiate a broad workup. However, soon after initial evaluation, you are called back into the room. The patient’s vitals are as follows and concerning for septic shock and an alarming serum sodium level.
An 82-year-old female is brought into the Emergency Department by family for a several day history of progressive altered mental status. You initiate a broad workup. However, soon after initial evaluation, you are called back into the room. The patient’s vitals are as follows and concerning for septic shock and an alarming serum sodium level.
 Matthew Zuckerman, MD
Matthew Zuckerman, MD Derrick Lung, MD MPH
Derrick Lung, MD MPH Zlatan Coralic, PharmD
Zlatan Coralic, PharmD